If Restless Legs Syndrome is keeping you up at night, you can become trapped in a vicious circle of insomnia and discomfort. If your RLS causes you to lose sleep, then the fact that you’re not resting well exacerbates the condition.
While we don’t have a cure, we have beds to recommend that may help ease your RLS symptoms as you sleep. The best mattresses for restless legs syndrome, in our opinion, have low motion transfer, middle-of-the-road firmness, and features that accommodate a variety of sleeping positions. Symptoms of restless legs syndrome sometimes go away after treating an underlying condition, such as iron deficiency. If you have RLS without an associated condition, treatment focuses on lifestyle changes. If those aren’t effective, your healthcare professional may prescribe medicines.
Take a look at our top picks below.
10 Best Mattresses for Restless Legs Syndrome
- Helix Midnight Luxe – Best Mattress for Combination Sleepers with Restless Legs Syndrome
- WinkBed – Best Hybrid Mattress for Restless Legs Syndrome
- Bear Star Hybrid – Best Mattress for Side Sleepers with Restless Legs Syndrome
- Saatva Classic – Best Mattress for Restless Legs Syndrome and Back Pain
- Nolah Signature – Best Mattress for Pressure Relief with Restless Legs Syndrome
- Brooklyn Bedding Signature Hybrid – Best Mattress for Back Sleepers with Restless Legs Syndrome
- DreamCloud – Best Luxury Mattress for Restless Legs Syndrome
- Nectar – Best Mattress for Couples with Restless Legs Syndrome
- Loom & Leaf – Best Memory Foam Mattress for Restless Legs Syndrome
- TEMPUR-Adapt® ProAdapt® – Best Mattress for Hip Pain with Restless Legs Syndrome
Compare The Best Mattresses for Restless Legs Syndrome
|

|

|

|

|

|

|

|

|

|
|
| Helix Midnight Luxe Mattress | WinkBed Mattress | Bear Star Hybrid Mattress | Saatva Mattress | Nolah Signature 12″ Mattress | Brooklyn Bedding Signature Hybrid Mattress | DreamCloud Original Mattress | Nectar Mattress | Loom & Leaf Mattress | TEMPUR-Adapt Mattress | |
| Rating | ||||||||||
| Firmness | Medium-firm: 6/10 | Multiple firmness options | Medium-firm: 6/10 | Multiple firmness options | Soft: 4/10 | Multiple firmness options | Medium-firm: 6.5/10 | Medium-firm: 6.5/10 | Multiple firmness options | |
| Material | Hybrid | Hybrid | Hybrid | Innerspring | Foam | Hybrid | Hybrid | Foam | Foam | Foam |
| Cooling | — |
|
|
|
— | — |
|
— | — |
|
| Warranty | 15-year warranty | Lifetime warranty | Lifetime warranty | Lifetime warranty | Lifetime warranty | 10-year warranty | Lifetime warranty | Lifetime warranty | Lifetime warranty | 10-year warranty |
| Shipping | Free shipping | Free shipping | Free shipping | Free white glove delivery | Free shipping | Free shipping | Free shipping | Free shipping | Free shipping | Free white glove delivery |
| Trial Period | 100 nights | 120 nights | 120 nights | 365 nights | 120 nights | 120 nights | 365 nights | 365 nights | 365 nights | 90 nights |
| Best For | Back Sleepers, Stomach Sleepers, Side Sleepers | Back Sleepers, Stomach Sleepers, Back Pain, Hot Sleepers, Side Sleepers | Joint Pain, Side Sleepers, Back Sleepers, Hot Sleepers | Back Sleepers, Stomach Sleepers, Back Pain, Hot Sleepers | Side Sleepers, Back Pain | Couples, Back Sleepers | Back Sleepers, Hot Sleepers, Seniors | Back Sleepers, Side Sleepers, Hip Pain, Joint Pain | Back Pain, Side Sleepers | Back Sleepers, Hot Sleepers |
Sleep Advisor’s Testing Methodology
At Sleep Advisor, our mattress reviews are based on findings from in-person tests that allow us to have a genuine understanding of how the mattress feels and performs. We look at features that are valuable to consumers, such as temperature control, bounce, edge support, and motion isolation.
We also evaluate mattress performance for back, side, and stomach sleeping. Lying in different positions lets us know how supportive the bed is and if it’s good at relieving pressure.
We then take all the information we’ve gathered to rate the bed in specific categories. These results allow us to help our readers find the right mattress for their needs.

Advice from a Medical Expert
We reached out to Dr. Raj Dasgupta, who has over 20 years of experience in the medical field, to see his thoughts on what key qualities people with restless legs syndrome should look for in a mattress.
“A mattress can not directly help restless leg syndrome. However, in general it is important to look for a mattress that’s comfortable, supportive, and relieves pressure on your legs without overheating, so you can sleep better and ease those symptoms.”
The Best Mattresses for Restless Legs Syndrome, Reviewed
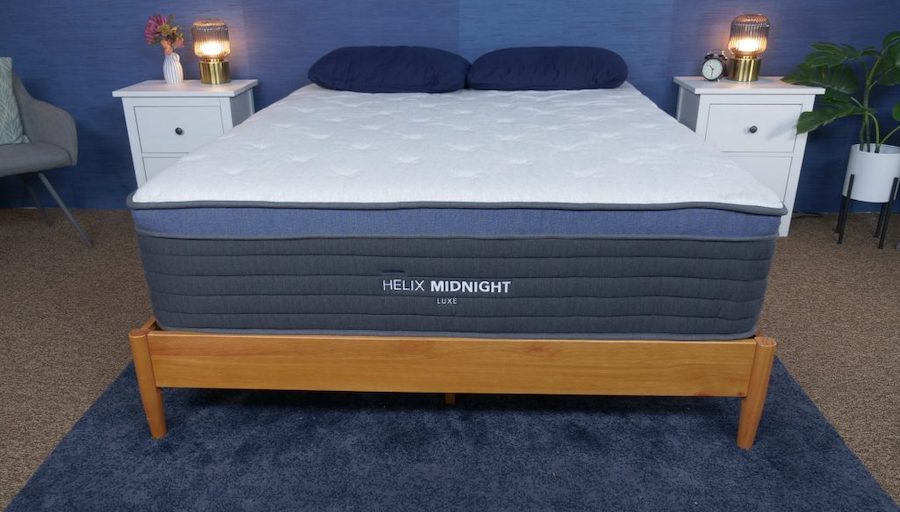
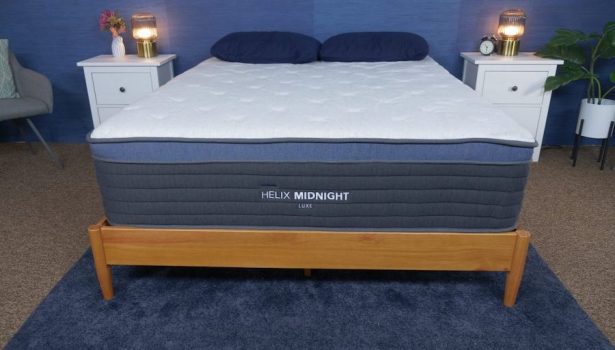
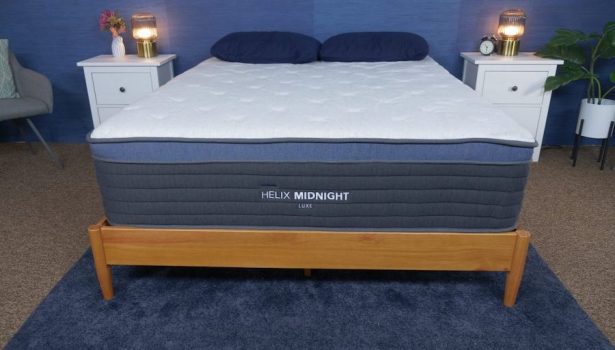
Helix Midnight Luxe – Best Mattress for Combination Sleepers with Restless Legs Syndrome
Helix Midnight Luxe Mattress
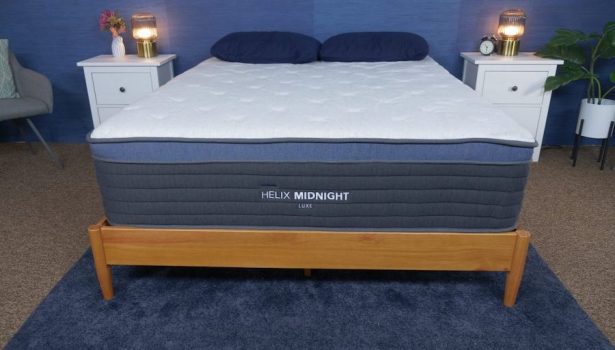
With the Ultra-Cool phase-changing cover and gel-infused foam, the Helix Midnight Luxe is an excellent choice for hot sleepers who also need pressure relief and zoned support.
Material
Hybrid
Trial Period
100 nights
Shipping Method
Free shipping
Firmness
Medium-firm: 6/10
Warranty
15-year warranty
Price Range
$$$$$
We recommend this mattress for the following sleeper types:
Back Sleeping
Ideal for average weight and heavyweight back sleepers.Side Sleeping
Ideal for average weight and heavyweight side sleepers.Stomach Sleeping
Ideal for lightweight stomach sleepers.Financing Options
Financing options are available for this mattress.
Helix Midnight Luxe Mattress
With the Ultra-Cool phase-changing cover and gel-infused foam, the Helix Midnight Luxe is an excellent choice for hot sleepers who also need pressure relief and zoned support.
Material
Hybrid
Warranty
15-year warranty
Firmness
Medium-firm: 6/10
Shipping Method
Free shipping
Trial Period
100 nights
Price Range
$$$$$
We recommend this mattress for the following sleeper types:
Back Sleeping
Ideal for average weight and heavyweight back sleepers.Side Sleeping
Ideal for average weight and heavyweight side sleepers.Stomach Sleeping
Ideal for lightweight stomach sleepers.Financing Options
Financing options are available for this mattress.
Helix Midnight Luxe Mattress
With the Ultra-Cool phase-changing cover and gel-infused foam, the Helix Midnight Luxe is an excellent choice for hot sleepers who also need pressure relief and zoned support.
Material
Hybrid
Firmness
Medium-firm: 6/10
Trial Period
100 nights
Warranty
15-year warranty
Shipping Method
Free shipping
Price Range
$$$$$
We recommend this mattress for the following sleeper types:
Back Sleeping
Ideal for average weight and heavyweight back sleepers.Side Sleeping
Ideal for average weight and heavyweight side sleepers.Stomach Sleeping
Ideal for lightweight stomach sleepers.Financing Options
Financing options are available for this mattress.
Why the Helix Midnight Luxe Earned Best Mattress for Combination Sleepers with Restless Legs Syndrome
The Midnight Luxe from Helix is an upgraded version of the brand’s Midnight mattress, one of our favorites here at Sleep Advisor. The Luxe edition has an additional layer of gel Visco foam that should help restless legs find soothing comfort.
The innerspring unit should provide good responsiveness for combination sleepers, making switching positions a breeze. The zoning in the coils further provides extra support in heavier areas like the midsection.
What’s the Helix Midnight Luxe Made Of?
The Helix Midnight Luxe is 13.5 inches tall and composed of six layers. All foams used in the mattress are CertiPUR-US® certified.

- Layer 1 – Premium Cooling Pillow Top. Choose between a standard Tencel™ cover or a Glaciotex™ cooling cover for even more temperature regulation in this comfortable, cushiony top layer.
- Layer 2 – Helix Responsive Foam. An adaptable layer of memory foam gives you support and some bounce.
- Layer 3 – Copper Gel Memory Foam. This foam contours to your body while the copper gel inside it diverts excess heat away.
- Layer 4 – Memory Plus Foam. A denser foam transitions into the coil layer below.
- Layer 5 – Coil Unit. Individually wrapped coils are zoned to support the areas of your body that need it most, like the lower back.
- Layer 6 – DuraDense Foam. Dense foam makes up the base of the mattress and ensures stability for the coils and other layers above.
Our Take: “If you’ve got the extra cash to spend, and you want enhanced support, cushioning up top, and cooling, then the Luxe is worth it.” – Emma Mattei, Sleep Advisor Mattress Tester
What We Liked
- Breathable – The Helix Midnight Luxe’s hybrid construction allows for air to flow through the coils within the mattress, making it a great choice for folks who sleep hot.
- Works for a lot of positions – The bed has a medium-firm feel and plenty of added features that should benefit a wide range of body types and sleeping positions. This versatility is also a big advantage for those with RLS, as they often shift around a lot at night.
Potential Drawbacks
- Too soft for some – Despite the Helix Midnight Luxe’s broad appeal, heavier folks or people who prefer to sleep on their stomachs might benefit more from something firmer.
- Hefty – We noticed that this bed was heavy and hard to move, since it’s lacking any handles or other features designed for easy transportation.
Customer Reviews of the Helix Midnight Luxe
On Helix’s website, the mattress scores 4.5 out of 5 stars. Customers appreciate the Helix Midnight Luxe mattress for its customized support but have reported that it may not be the best option for those who prefer an exceptionally soft sleep surface.
Want to know more? See our full Helix Midnight Luxe mattress review or explore our top picks for the best mattresses for combination sleepers.
WinkBed – Best Hybrid Mattress for Restless Legs Syndrome
WinkBed Mattress

WinkBed is a luxury hybrid bed with a variety of comfort features that should make it a versatile pick for most sleeping positions.
Material
Hybrid
Trial Period
120 nights
Shipping Method
Free shipping
Firmness
Multiple firmness options
Warranty
Lifetime warranty
Price Range
$$$$$
We recommend this mattress for the following sleeper types:
Hot Sleepers
If you often overheat while you sleep, this mattress should help you stay cool.Back Pain
This bed is perfect for anyone suffering from back pain.Back Sleeping
Ideal for lightweight and average weight back sleepers.Side Sleeping
Ideal for lightweight and average weight side sleepers.Stomach Sleeping
Ideal for average weight stomach sleepers.Financing Options
Financing options are available for this mattress.
WinkBed Mattress

WinkBed is a luxury hybrid bed with a variety of comfort features that should make it a versatile pick for most sleeping positions.
Material
Hybrid
Warranty
Lifetime warranty
Firmness
Multiple firmness options
Shipping Method
Free shipping
Trial Period
120 nights
Price Range
$$$$$
We recommend this mattress for the following sleeper types:
Hot Sleepers
If you often overheat while you sleep, this mattress should help you stay cool.Back Pain
This bed is perfect for anyone suffering from back pain.Back Sleeping
Ideal for lightweight and average weight back sleepers.Side Sleeping
Ideal for lightweight and average weight side sleepers.Stomach Sleeping
Ideal for average weight stomach sleepers.Financing Options
Financing options are available for this mattress.

WinkBed Mattress
WinkBed is a luxury hybrid bed with a variety of comfort features that should make it a versatile pick for most sleeping positions.
Material
Hybrid
Firmness
Multiple firmness options
Trial Period
120 nights
Warranty
Lifetime warranty
Shipping Method
Free shipping
Price Range
$$$$$
We recommend this mattress for the following sleeper types:
Hot Sleepers
If you often overheat while you sleep, this mattress should help you stay cool.Back Pain
This bed is perfect for anyone suffering from back pain.Back Sleeping
Ideal for lightweight and average weight back sleepers.Side Sleeping
Ideal for lightweight and average weight side sleepers.Stomach Sleeping
Ideal for average weight stomach sleepers.Financing Options
Financing options are available for this mattress.
Why the WinkBed Earned Best Hybrid Mattress for Restless Legs Syndrome
The WinkBed mattress features a considered and sturdy design that includes a breathable Tencel™ cover, gel-infused foam, support foams, and an innerspring unit.
It comes in three firmness options, and the added customization could make it easier for you to sleep if you’re dealing with restless legs. While the soft version is best for side sleepers and lightweight individuals, the luxury firm and firm models are better for stomach sleepers, back sleepers, and average to heavier people.
What’s the WinkBed Made Of?
The WinkBed comes in four firmness options: Softer, Luxury Firm, Firmer, and Plus (for shoppers over 200 pounds). It stands 13.5 inches tall.
- Tencel™ Cover. Soft and moisture-wicking for a breathable, dry, and comfortable sleep surface.
- Euro Pillow Top. Cushions and conforms to the body with gel-infused foams for added cooling ability.
- Transitional Foam Layers. A series of foam layers help support the sleeper above while also dampening the feel of the coils below.
- Coil Layer. Individually wrapped coils are zoned to bolster support or offer more give where necessary for proper alignment.

Our Take: “People who like to feel like they are sleeping in the bed may feel more like they are floating on top of this mattress, but there should be plenty of pressure relief to make up for that.” – Sean, Sleep Advisor Mattress Tester
What We Liked
- Certified safe – The WinkBed has OEKO-TEX® and CertiPUR-US® certifications, which means the mattress meets strict health and safety standards.
- Customizable – Four total firmness options that include one specifically for plus-sized folks? It’s difficult to find mattresses that offer this level of variety. You should be able to find something that works for your tastes while enabling some relief from restless legs syndrome.
Potential Drawbacks
- Not the softest option – This bed’s sturdy hybrid construction gives it a firmer feel and doesn’t lend itself well to the cradling and “hugging” sensations distinctive of all-foam mattresses.
- Some movement carries – The foams on top of the WinkBed can prevent some motion from traveling across the mattress surface, but not very much. It’s still a hybrid bed with a springy profile.
Customer Reviews of the WinkBed mattress
On the WinkBeds site, the WinkBed earns a 4.8 out of 5 stars. One drawback of the WinkBed mattress is that it might be too expensive for budget-conscious shoppers, but overall it offers excellent durability and customizable firmness options.
Interested in more details? View our WinkBeds mattress review or discover more hybrid mattresses.
Bear Star Hybrid – Best Mattress for Side Sleepers with Restless Legs Syndrome
Bear Star Hybrid Mattress

The Bear Hybrid is an appealing product because it should cater to a wide variety of sleepers.
Material
Hybrid
Trial Period
120 nights
Shipping Method
Free shipping
Firmness
Medium-firm: 6/10
Warranty
Lifetime warranty
Price Range
$$$$$
We recommend this mattress for the following sleeper types:
Hot Sleepers
If you often overheat while you sleep, this mattress should help you stay cool.Joint Pain
This bed is perfect for anyone suffering from joint pain.Back Sleeping
Ideal for lightweight back sleepers.Side Sleeping
Ideal for average weight side sleepers.Financing Options
Financing options are available for this mattress.
Bear Star Hybrid Mattress

The Bear Hybrid is an appealing product because it should cater to a wide variety of sleepers.
Material
Hybrid
Warranty
Lifetime warranty
Firmness
Medium-firm: 6/10
Shipping Method
Free shipping
Trial Period
120 nights
Price Range
$$$$$
We recommend this mattress for the following sleeper types:
Hot Sleepers
If you often overheat while you sleep, this mattress should help you stay cool.Joint Pain
This bed is perfect for anyone suffering from joint pain.Back Sleeping
Ideal for lightweight back sleepers.Side Sleeping
Ideal for average weight side sleepers.Financing Options
Financing options are available for this mattress.

Bear Star Hybrid Mattress
The Bear Hybrid is an appealing product because it should cater to a wide variety of sleepers.
Material
Hybrid
Firmness
Medium-firm: 6/10
Trial Period
120 nights
Warranty
Lifetime warranty
Shipping Method
Free shipping
Price Range
$$$$$
We recommend this mattress for the following sleeper types:
Hot Sleepers
If you often overheat while you sleep, this mattress should help you stay cool.Joint Pain
This bed is perfect for anyone suffering from joint pain.Back Sleeping
Ideal for lightweight back sleepers.Side Sleeping
Ideal for average weight side sleepers.Financing Options
Financing options are available for this mattress.
Why the Bear Star Hybrid Earned Best Mattress for Side Sleepers with Restless Legs Syndrome
Side sleepers with restless legs syndrome will want an extra-comfy bed to help them sleep easier. Bear offers a solution with their Hybrid mattress.
Aside from foam layers, on top of the mattress is a unique cover made with Celliant®, an innovative textile that may encourage post-exercise recovery by reducing inflammation and boosting circulation. It’s unclear whether Celliant® could improve RLS symptoms, but as it’s geared toward helping muscles recuperate, we think it’s certainly worth a shot. Thankfully, Bear gives you 120 nights to try out the bed at home to see if you notice an improvement.
What’s the Bear Star Hybrid Made Of?
At 13 inches tall, the Bear Star Hybrid has a total of five layers.
Layer 1 – Cover. The cover feels cool, thanks to a combination of HydroCool® technology and Celliant® fibers.
Layer 2 – Serene Gel Foam. This gel-infused foam provides pressure relief with even more cooling capability.
Layer 3 – Responsive Comfort Foam. This next layer is more responsive and therefore adapts to your body as you switch positions.

Layer 4 – Innerspring Unit. The spring layer is made up of individually wrapped coils for targeted support. They’re stronger around the perimeter of the mattress for reinforced edges.
Layer 5 – High-Density Support Foam. The mattress sits on top of a base of dense foam.
Our Take: “The Bear Star mattress has a unique five-layer design that provides exceptional pressure relief and support for all sleeping positions.” – Stuart Petty, Sleep Advisor Mattress Tester
What We Liked
Cool textile – Celliant®, found in the cover of the Bear Star Hybrid, is a unique fiber that’s said to aid in muscle recovery by converting excess body heat into infrared energy. So not only might it help keep the surface of the mattress cool, active sleepers may benefit from its healing capabilities.
Plenty certified – The Bear Star Hybrid boasts a number of certifications for safety when it comes to the materials in its construction. It’s GREENGUARD Gold certified for low emissions and promotes the preservation of clean air. All its foams are also CertiPUR-US® certified to ensure health and safety.
Potential Drawbacks
- Can feel too firm – If you’re a petite sleeper, there’s a chance the Bear Star Hybrid may feel a bit too unyielding for noticeable pressure relief.
- Lacking edge support – During testing, Stuart found the edges of the bed weren’t super strong, meaning folks who like to lay or sit on the perimeter of their mattress could end up sinking.
Customer Reviews of the Bear Star Hybrid
Coming in at approximately 4.5 out of 5 stars on Bear’s site, a potential downside customers noted of the Bear Star Hybrid mattress is that some users may find it too firm, but it is praised for its strong support and cooling properties, promoting a comfortable sleep environment.
Interested in more details? View our guide to the Bear Star Hybrid mattress. Check out our best mattresses for side sleepers too!
Saatva Classic – Best Mattress for Restless Legs Syndrome and Back Pain
Saatva Mattress

Coil-on-coil structure gives this elevated innerspring bed a luxurious feel and versatility.
Material
Innerspring
Trial Period
365 nights
Shipping Method
Free white glove delivery
Firmness
Multiple firmness options
Warranty
Lifetime warranty
Price Range
$$$$$
We recommend this mattress for the following sleeper types:
Hot Sleepers
If you often overheat while you sleep, this mattress should help you stay cool.Back Pain
This bed is perfect for anyone suffering from back pain.Back Sleeping
Ideal for lightweight, average weight, and heavyweight back sleepers.Stomach Sleeping
Ideal for lightweight and average weight stomach sleepers.Financing Options
Financing options are available for this mattress.
Saatva Mattress

Coil-on-coil structure gives this elevated innerspring bed a luxurious feel and versatility.
Material
Innerspring
Warranty
Lifetime warranty
Firmness
Multiple firmness options
Shipping Method
Free white glove delivery
Trial Period
365 nights
Price Range
$$$$$
We recommend this mattress for the following sleeper types:
Hot Sleepers
If you often overheat while you sleep, this mattress should help you stay cool.Back Pain
This bed is perfect for anyone suffering from back pain.Back Sleeping
Ideal for lightweight, average weight, and heavyweight back sleepers.Stomach Sleeping
Ideal for lightweight and average weight stomach sleepers.Financing Options
Financing options are available for this mattress.

Saatva Mattress
Coil-on-coil structure gives this elevated innerspring bed a luxurious feel and versatility.
Material
Innerspring
Firmness
Multiple firmness options
Trial Period
365 nights
Warranty
Lifetime warranty
Shipping Method
Free white glove delivery
Price Range
$$$$$
We recommend this mattress for the following sleeper types:
Hot Sleepers
If you often overheat while you sleep, this mattress should help you stay cool.Back Pain
This bed is perfect for anyone suffering from back pain.Back Sleeping
Ideal for lightweight, average weight, and heavyweight back sleepers.Stomach Sleeping
Ideal for lightweight and average weight stomach sleepers.Financing Options
Financing options are available for this mattress.
Why the Saatva Classic Earned Best Mattress for Restless Legs Syndrome and Back Pain
If you’re looking for lumbar support as a defense against back pain, the Saatva Classic is an extremely good bet. It has lumbar-targeting elements in its Euro pillow top, its foam layer, and both—yes, both—of its spring units.
This luxury mattress should also prove helpful for sleepers with Restless Legs Syndrome, as it’s available in three different firmness levels and, as I observed during testing, provides a “Goldilocks-esque” ratio of softness to support.
What’s the Saatva Classic Made Of?
The Saatva Classic is available in three firmnesses (Plush Soft, Luxury Firm, and Firm) and two heights (11.5 or 14.5 inches).
- Euro Pillow Top. The top of the mattress has a soft, cushioning feel and an antimicrobial treatment on its breathable organic cotton cover.
- Lumbar Crown. A specialized strip of CertiPUR-US® certified foam supports the lower back area.
- First Coil Layer. Zoned coils ensure proper give and lift in the right places, balancing bouncy support and pressure relief.

- Spinal Wire. Found within the two coil units, the Lumbar Zone® Active Spinal Wire braces the lumbar region to promote healthy alignment of the body.
- Second Coil Layer. More coils beneath the first unit give the Saatva Classic impressive durability and allow for even more airflow throughout the mattress.
- Foam Rails. Around the perimeter of the mattress, there’s a layer of high-density foam rails for enhanced edge support.
My Take: If you deal with back pain, the Saatva Classic has you covered with numerous features that target the lower back. There’s extra lumbar support in the soft Euro pillow top, plus two different layers of coils and a “Spinal Wire” that keep the lower back lifted.
What I Liked
- Customizable – Not only can you select your favorite firmness level from a set of three choices, but you can also pick the height of your mattress: The Saatva Classic is available in 14.5- and 11.5-inch models.
- White glove delivery – One of my favorite things about Saatva is their white glove delivery policy. They’ll send workers to your house to remove your old mattress and install your new one—all for free.
Potential Drawbacks
- Returns cost extra – Despite the hassle-free delivery, it should be noted that Saatva will charge you $99 to return a mattress, even if you send it back within the trial period.
- Not the best motion isolation – Two spring units mean double the bounciness, but also double the motion transfer. You’re likely to feel your partner moving around on the other side of the bed.
Customer Reviews of the Saatva Classic
The Saatva Classic rates 4.8 stars out of 5 on Saatva’s website. One negative aspect customers found with the Saatva Classic mattress is that it may feel too firm for some users, while a notable advantage is its high-quality materials, providing durability and support.
Interested in this bed? See our full Saatva mattress review or peruse our roundup of the best mattresses for back pain.
Nolah Signature – Best Mattress for Pressure Relief with Restless Legs Syndrome
Nolah Signature 12″ Mattress

Shoppers interested in a hybrid feel should find this Signature bed a perfect choice for their needs.
Material
Foam
Trial Period
120 nights
Shipping Method
Free shipping
Firmness
Soft: 4/10
Warranty
Lifetime warranty
Price Range
$$$$$
Nolah Signature 12″ Mattress

Shoppers interested in a hybrid feel should find this Signature bed a perfect choice for their needs.
Material
Foam
Warranty
Lifetime warranty
Firmness
Soft: 4/10
Shipping Method
Free shipping
Trial Period
120 nights
Price Range
$$$$$

Nolah Signature 12″ Mattress
Shoppers interested in a hybrid feel should find this Signature bed a perfect choice for their needs.
Material
Foam
Firmness
Soft: 4/10
Trial Period
120 nights
Warranty
Lifetime warranty
Shipping Method
Free shipping
Price Range
$$$$$
Why the Nolah Signature Earned Best Mattress for Pressure Relief with Restless Legs Syndrome
The Nolah Signature is rated 4 out of 10 on our Sleep Advisor firmness scale, making this bed an excellent fit for anyone looking for plushness and quality pressure relief. It also isolates motion well, so if you have restless legs syndrome, you’re less likely to disturb your partner when you move.
Nolah’s proprietary AirFoam™ is made to contour like traditional memory foam while staying cool, since overheating is a common drawback of classic memory materials. The Signature includes two layers of AirFoam™, with the second layer delivering advanced pressure relief.
What’s the Nolah Signature Made Of?
The Nolah Signature is 12 inches tall with five layers.
- Layer 1 – Organic Cotton Cover. A breathable and dry surface that feels super soft.
- Layer 2 – Plush Nolah AirFoam™ (2.5 inches). AirFoam™ has an open-pored construction to allow for more airflow, and this layer also contours to and cushions your body.
- Layer 3 – Active Response Foam (1.5 inches). This responsive foam readily adapts to shifts in your sleeping position.
- Layer 4 – Firm Nolah AirFoam™ (1 inch). A firmer Nolah AirFoam™ balances support and pressure relief.
- Layer 5 – Core Foundation (7 inches). High-density foam gives the bed its durable stability.
Our Take: “The Nolah Signature is a softer mattress, so it’s going to excel for side sleepers who want pressure relief in their shoulders and hips.” – Emma, Sleep Advisor Mattress Tester
What We Liked
- Pressure-relieving – It’s no wonder the Nolah Signature is a match for side sleepers: Its soft foam layers cradle and cushion problem areas with ease, all while its dense core at the bottom maintains support.
- Surprisingly cooling for an all-foam bed – Memory foam has a reputation for trapping heat, but Nolah’s AirFoam™ seeks to reduce that downside. Emma noted that the bed has “a much cooler feel” than traditional foam mattresses.
Potential Drawbacks
- Too soft for some – The Nolah’s softer feel is ideal for pressure relief, but most stomach sleepers will probably find this bed too plush to support them properly.
- Lackluster edges – There’s no special reinforcement around the perimeter of the Nolah Signature, and we noticed that the edges sagged when sitting on them. Laying on or near the edges didn’t seem to be as much of a problem, though.
Customer Reviews of the Nolah Signature
The Nolah Signature gets a 4.8 out of 5 stars on Nolah’s website. One potential drawback of the Nolah Signature mattress is its limited firmness options, but it excels in providing exceptional pressure relief and a cooling sleep experience.
Interested in more details? View our complete guide to the Nolah Signature mattress.
Brooklyn Bedding Signature Hybrid – Best Mattress for Back Sleepers with Restless Legs Syndrome
Brooklyn Bedding Signature Hybrid Mattress

The Brooklyn Bedding Signature Hybrid is priced similarly to other bed-in-the-box options, it represents a fantastic value in the hybrid market.
Material
Hybrid
Trial Period
120 nights
Shipping Method
Free shipping
Firmness
Multiple firmness options
Warranty
10-year warranty
Price Range
$$$$$
Brooklyn Bedding Signature Hybrid Mattress

The Brooklyn Bedding Signature Hybrid is priced similarly to other bed-in-the-box options, it represents a fantastic value in the hybrid market.
Material
Hybrid
Warranty
10-year warranty
Firmness
Multiple firmness options
Shipping Method
Free shipping
Trial Period
120 nights
Price Range
$$$$$

Brooklyn Bedding Signature Hybrid Mattress
The Brooklyn Bedding Signature Hybrid is priced similarly to other bed-in-the-box options, it represents a fantastic value in the hybrid market.
Material
Hybrid
Firmness
Multiple firmness options
Trial Period
120 nights
Warranty
10-year warranty
Shipping Method
Free shipping
Price Range
$$$$$
Why the Brooklyn Bedding Signature Hybrid Earned Best Mattress for Back Sleepers with Restless Legs Syndrome
If you’re dealing with restless legs syndrome, you’ll want a mattress that feels comfortable enough to help you get to sleep quickly. For those who sleep on their backs, a hybrid model like the Brooklyn Bedding Signature Hybrid could give you the right balance of pressure relief and support that most back sleepers need.
The Brooklyn Bedding Signature Hybrid comes in three firmness levels: Soft, Medium, and Firm. This customization is especially beneficial to those with RLS because it helps ensure the bed more closely meets their personal standards for comfort.
What’s the Brooklyn Bedding Signature Hybrid Made Of?
The Brooklyn Bedding Signature Hybrid comes in three firmnesses: Soft, Medium, or Firm. We’re going to describe the Medium model as the middle-of-the-road option. It houses five total layers inside its 11.5-inch tall construction.
- Layer 1 – Quilted Top (1 inch). A comfortable sleep surface that relieves pressure while resisting lasting indentations made by the sleeper’s body.
- Layer 2 – Supreme Response Comfort Foam (1.5 inches). A flexible, springy foam that adjusts to the sleeper’s movements.
- Layer 3 – VariFlex™ Transition Foam (1 inch). This foam provides pressure relief without allowing you to sink too far into the mattress.

- Layer 4 – Ascension® Coil Unit (8 inches). Coils react individually to offer support where it’s needed while also dampening motion transfer.
- Layer 5 – Flex Base (0.25 inches). The base reinforces the coils above it along with the rest of the mattress.
Our Take: “We think this bed would be great for combination sleepers. Because it’s so responsive, adjusting positions is super easy. Plus, with the supportive yet comfortable feel, this bed is super versatile for all sleeping positions.” – Emma, Sleep Advisor Mattress Tester
What We Liked
- Something for everyone – While the Medium model of the Brooklyn Bedding Signature Hybrid will likely be best for the majority of people, those who skew on the lighter or heavier side in terms of body weight might find the Soft or Firm versions more appealing, respectively.
- Bouncy – The coils in this hybrid are beyond responsive. Folks with restless legs should have no problems moving and switching positions on its surface.
Potential Drawbacks
- Too firm for some – Back sleepers should be set on this bed, but if you’re a lightweight sleeper or happen to switch to your side throughout the night, you might find the Brooklyn Bedding Signature Hybrid’s lack of cradling foams a bit uncomfortable.
- No bells or whistles – The Brooklyn Bedding Signature Hybrid is pretty simple, which isn’t necessarily a bad thing—it still checks all the boxes for your basic mattress functions. However, shoppers looking for something with more frills can definitely find fancier beds on this list.
Customer Reviews of the Brooklyn Bedding Signature Hybrid
On Brooklyn Bedding’s website, the Brooklyn Signature has 4.7 out of 5 stars. The Brooklyn Bedding Signature Hybrid mattress receives praise from customers for its versatility with different firmness options, but some have mentioned that it may produce slight noise when bearing weight.
Interested in learning more? Read our full-length Brooklyn Bedding Signature Hybrid review, or discover our top picks for the best mattresses for back sleepers.
DreamCloud – Best Luxury Mattress for Restless Legs Syndrome
DreamCloud Original Mattress

Luxurious hybrid at a great price with a lifetime warranty.
Material
Hybrid
Trial Period
365 nights
Shipping Method
Free shipping
Firmness
Medium-firm: 6.5/10
Warranty
Lifetime warranty
Price Range
$$$$$
We recommend this mattress for the following sleeper types:
Hot Sleepers
If you often overheat while you sleep, this mattress should help you stay cool.Seniors
This bed is perfect for senior sleepers.Back Sleeping
Ideal for average weight back sleepers.Financing Options
Financing options are available for this mattress.
DreamCloud Original Mattress

Luxurious hybrid at a great price with a lifetime warranty.
Material
Hybrid
Warranty
Lifetime warranty
Firmness
Medium-firm: 6.5/10
Shipping Method
Free shipping
Trial Period
365 nights
Price Range
$$$$$
We recommend this mattress for the following sleeper types:
Hot Sleepers
If you often overheat while you sleep, this mattress should help you stay cool.Seniors
This bed is perfect for senior sleepers.Back Sleeping
Ideal for average weight back sleepers.Financing Options
Financing options are available for this mattress.

DreamCloud Original Mattress
Luxurious hybrid at a great price with a lifetime warranty.
Material
Hybrid
Firmness
Medium-firm: 6.5/10
Trial Period
365 nights
Warranty
Lifetime warranty
Shipping Method
Free shipping
Price Range
$$$$$
We recommend this mattress for the following sleeper types:
Hot Sleepers
If you often overheat while you sleep, this mattress should help you stay cool.Seniors
This bed is perfect for senior sleepers.Back Sleeping
Ideal for average weight back sleepers.Financing Options
Financing options are available for this mattress.
Why the DreamCloud Earned Best Luxury Mattress for Restless Legs Syndrome
DreamCloud is a preferred recommendation at Sleep Advisor because it delivers luxury at an attainable price. Its construction features memory and poly foams to help absorb motion while providing comfort and support. Folks with restless leg syndrome should also appreciate the lifted and responsive surface.
The bed also uses individually wrapped coils, further minimizing motion transfer while also giving the bed more bounce for ease of movement—a great combination if you or your partner has restless legs.
What’s the DreamCloud Made Of?
The DreamCloud mattress has seven layers that make up its 14-inch profile. All of the foams within it are also CertiPUR-US® certified.
- Layer 1 – Cashmere Blend Cover. A soft and luxurious surface to sleep on.
- Layer 2 – Plush Soft Foam (1.5 inches). This foam is stitched into the cover, and it cushions your body while simultaneously offering a bit of support.
- Layer 3 – Gel-Infused Memory Foam (1 inch). This foam provides pressure relief by contouring to your body’s curves.

- Layer 4 – Standard Foam (2 inches). A transition layer that supports alignment and dampens the feel of coils beneath.
- Layer 5 – Coil Unit (8.5 inches). Steel coils allow for airflow while responding individually to mitigate motion transfer. The perimeter has thicker coils for stronger edges.
- Layer 6 – Base Layer (1 inch). Dense foam supports the layers on top while giving stability to the overall mattress.
- Layer 7 – Shift-Resistant Lower Cover. The lower cover helps the layers of the bed stay in place and sports handles for easy transportation.
My Take: The DreamCloud is one of my favorites. It’s a well-rounded bed that has luxury features without the high price tag. It should do well for anyone who wants a springy, supportive bed with a stately height.
What I Liked
- Lifted feeling – You’re going to feel like you’re lying on top of this mattress, rather than sinking into it. I think this supportive feeling is a plus for restless sleepers who need ease of movement.
- Reasonable price – With luxury features and a durable construction, I’m surprised the DreamCloud doesn’t cost more. It’s only around $1,300 for a queen.
Potential Drawbacks
- Not so soft – As a stomach sleeper, I found this bed to have the right amount of support and lift, but that’s not going to work for everyone. Side sleepers who need pressure relief or lightweight folks who struggle to sink into mattress surfaces should consider something softer.
- So-so edge support – Despite the DreamCloud having some reinforcement built into its construction, when I sat on the perimeter of the bed, it didn’t hold me up as well as I would have liked.
Customer Reviews of the DreamCloud mattress
The DreamCloud Original scores a solid 4.7 out of 5 stars among customers on its site. While some customers appreciate the value and affordability of the DreamCloud Original mattress, others find it to be on the heavier side, which could make moving or rotating the mattress more challenging.
Need more info? Read our complete DreamCloud mattress review or browse the best luxury mattresses.
Nectar – Best Mattress for Couples with Restless Legs Syndrome
Nectar Mattress

Nectar offers the deeper hug of a traditional memory foam bed but with updated cooling and a Forever warranty.
Material
Foam
Trial Period
365 nights
Shipping Method
Free shipping
Firmness
Medium-firm: 6.5/10
Warranty
Lifetime warranty
Price Range
$$$$$
We recommend this mattress for the following sleeper types:
Joint Pain
This bed is perfect for anyone suffering from joint pain.Hip Pain
This bed is perfect for anyone suffering from hip pain.Back Sleeping
Ideal for lightweight and average weight back sleepers.Side Sleeping
Ideal for lightweight and average weight side sleepers.Financing Options
Financing options are available for this mattress.
Nectar Mattress

Nectar offers the deeper hug of a traditional memory foam bed but with updated cooling and a Forever warranty.
Material
Foam
Warranty
Lifetime warranty
Firmness
Medium-firm: 6.5/10
Shipping Method
Free shipping
Trial Period
365 nights
Price Range
$$$$$
We recommend this mattress for the following sleeper types:
Joint Pain
This bed is perfect for anyone suffering from joint pain.Hip Pain
This bed is perfect for anyone suffering from hip pain.Back Sleeping
Ideal for lightweight and average weight back sleepers.Side Sleeping
Ideal for lightweight and average weight side sleepers.Financing Options
Financing options are available for this mattress.

Nectar Mattress
Nectar offers the deeper hug of a traditional memory foam bed but with updated cooling and a Forever warranty.
Material
Foam
Firmness
Medium-firm: 6.5/10
Trial Period
365 nights
Warranty
Lifetime warranty
Shipping Method
Free shipping
Price Range
$$$$$
We recommend this mattress for the following sleeper types:
Joint Pain
This bed is perfect for anyone suffering from joint pain.Hip Pain
This bed is perfect for anyone suffering from hip pain.Back Sleeping
Ideal for lightweight and average weight back sleepers.Side Sleeping
Ideal for lightweight and average weight side sleepers.Financing Options
Financing options are available for this mattress.
Why the Nectar Earned Best Mattress for Couples with Restless Legs Syndrome
The Nectar mattress should allow you to move your restless legs without feeling stuck or disturbing your partner too much. While traditional memory foams could make you feel hemmed in and overly warm, Nectar’s updates to this classic material make it more responsive and cooling than most all-foam mattresses.
Despite that, it still retains stellar motion-isolation to ensure sleep remains undisturbed throughout any tossing and turning, regardless of who’s doing it.
What’s the Nectar Made Of?
The Nectar mattress is 12 inches thick and has five layers when you include its upper and lower covers. All foams in the bed are also CertiPUR-US® certified.
- Layer 1 – Breathable Cooling Cover. Polyethylene fibers absorb excess heat for a cooler sleep surface.
- Layer 2 – Gel Memory Foam (2 inches). A more cooling foam that relieves pressure buildup in problem areas.
- Layer 3 – Dynamic Response Foam (3 inches). This bouncier foam transitions between the softer cradling foam above and the firmer base layer below.

- Layer 4 – ActiveSupport Base (7 inches). A thick base of foam gives the mattress its durable structure.
- Layer 5 – Shift-Resistant Lower Cover. A polyester cover that keeps your mattress in place.
My Take: The Nectar balances the conventional motion-isolating capabilities of memory foam with more noticeable responsiveness (or bounce-back), making it a great option for couples suffering from RLS. They’re going to need the ability to move around more easily without waking up their partner.
What I Liked
- Great policies – The company offers one of the most generous sleep trials on the current market, giving you a full year to decide if the Nectar is the perfect fit for you and your sleep needs. As an added bonus, there’s also a forever warranty.
- Motion begone – Nectar performs exceptionally well at motion isolation, a valuable feature for couples. Because its foams absorb the ripples and shakes that result from movement, your partner is less likely to wake up while you’re fidgeting.
Potential Drawbacks
- Not the coolest – Though the Nectar has some cooling tech infused into its cover and top layer, it’s still a dense all-foam bed, and those are notoriously prone to overheating. Sleepers who struggle with feeling hot at night should check out a hybrid bed or something with a dedicated cooling construction.
- Too soft for some – Heavier sleepers and those who prefer to lie on their stomachs might sink too far into the Nectar’s foam layers.
Customer Reviews of the Nectar mattress
With thousands of reviews on Nectar’s website, the Nectar mattress has an average 4.8 out of 5 stars. One common customer complaint about the Nectar mattress is its longer-than-average break-in period, while many customers praise its excellent value and comfort once fully settled.
Looking to learn more? Check out our full review for the Nectar mattress or check out our picks for the best mattresses for couples.
Loom & Leaf – Best Memory Foam Mattress for Restless Legs Syndrome
Loom & Leaf Mattress

Material
Foam
Trial Period
365 nights
Shipping Method
Free shipping
Firmness
Multiple firmness options
Warranty
Lifetime warranty
Price Range
$$$$$
Loom & Leaf Mattress

Material
Foam
Warranty
Lifetime warranty
Firmness
Multiple firmness options
Shipping Method
Free shipping
Trial Period
365 nights
Price Range
$$$$$

Loom & Leaf Mattress
Material
Foam
Firmness
Multiple firmness options
Trial Period
365 nights
Warranty
Lifetime warranty
Shipping Method
Free shipping
Price Range
$$$$$
Why the Loom & Leaf Earned Best Memory Foam Mattress for Restless Legs Syndrome
The Saatva Loom & Leaf mattress is a memory foam bed that defies convention. Its six layers elevate it above its fellow all-foam competitors, and two firmness options—Relaxed-Firm or Firm—allow you to pick precisely the right feel for your restless legs syndrome symptoms.
Most memory foam beds have far fewer than five distinct foam layers. The Loom & Leaf breaks the mold with specialized foams for pressure relief, support, stability, and cooling.
What’s the Loom & Leaf Made Of?
The Loom & Leaf by Saatva comes in two firmness options: Relaxed Firm or Firm. It’s 12 inches thick and has six total layers.
- Layer 1 – Cover. Made out of organic cotton and treated to resist microbes, this cover should feel soft and breathable.
- Layer 2 – Lumbar Crown. This layer only occupies the middle third of the mattress, right beneath your lower back, and is intended to boost support for that crucial area.
- Layer 3 – Gel-infused Foam (2 inches). Contouring, pressure-relieving foam that’s perforated for better airflow.
- Layer 4 – Memory Foam Core (2.5 inches). A denser foam for deeper support.
- Layer 5 – Transitional Foam (2 inches). A loft pad that acts as the buffer between the comfort and support layers.
- Layer 6 – Foam Base (5.5 inches). A stable, durable base layer of foam for support.
Our Take: “Overall, Loom & Leaf is soft and luxurious, but doesn’t sacrifice any support. If you’re looking for a memory foam bed that keeps you more cradled to the surface, you should love this brand.” – Stuart, Sleep Advisor Mattress Tester
What We Liked
- Green construction – Saatva’s knowledge of memory foam is well-balanced with a respect for eco-friendly features. The cover on this bed is made with organic cotton, and instead of a synthetic flame barrier, the Loom & Leaf has a plant-based thistle pulp one.
- White glove delivery – Saatva’s White Glove delivery policy means that you don’t need to set this bed up yourself. Simply tell the delivery team where you’d like it, and they’ll handle placement (as well as removal of your old mattress, if requested when you make your order).
Potential Drawbacks
- Pretty pricey – The Loom & Leaf is considered a luxury foam mattress, so it has a a higher price than many competitors. Before sales and coupons, a queen should cost you around $2,400.
- Not for heavier sleepers – Lighter and average-weight sleepers should find the support they need from the Loom & Leaf, but it’s possible that heavier sleepers might think it’s too soft.
Want to know more? See our full Loom & Leaf mattress review or explore our picks for the best memory foam mattresses.
TEMPUR-Adapt® ProAdapt® – Best Mattress for Hip Pain with Restless Legs Syndrome
TEMPUR-Adapt Mattress

The TEMPUR-Adapt® uses original TEMPUR® material to give sleepers enhanced pressure relief .
Read TEMPUR-Adapt Mattress ReviewMaterial
Foam
Trial Period
90 nights
Shipping Method
Free white glove delivery
Firmness
Medium-firm: 7/10
Warranty
10-year warranty
Price Range
$$$$$
TEMPUR-Adapt Mattress

The TEMPUR-Adapt® uses original TEMPUR® material to give sleepers enhanced pressure relief .
Read TEMPUR-Adapt Mattress ReviewMaterial
Foam
Warranty
10-year warranty
Firmness
Medium-firm: 7/10
Shipping Method
Free white glove delivery
Trial Period
90 nights
Price Range
$$$$$

TEMPUR-Adapt Mattress
The TEMPUR-Adapt® uses original TEMPUR® material to give sleepers enhanced pressure relief .
Read TEMPUR-Adapt Mattress ReviewMaterial
Foam
Firmness
Medium-firm: 7/10
Trial Period
90 nights
Warranty
10-year warranty
Shipping Method
Free white glove delivery
Price Range
$$$$$
Why the TEMPUR-Adapt Pro-Adapt Earned Best Mattress for Hip Pain with Restless Legs Syndrome
Hip pain combined with restless legs syndrome can quickly lead to sleepless nights. The TEMPUR-Adapt ProAdapt is a foam mattress designed for optimal comfort, offering shoppers four firmness choices.
Each ProAdapt® contains proprietary materials with slight variations among the models to create the desired feel. The comfort layers of these mattresses, particularly the Medium and Soft versions, should deliver soothing pressure relief around the hips. Meanwhile, the “Adapt” in the bed’s name should be a green flag to those with RLS, as it implies a mattress that can accommodate multiple sleeping positions.
What’s the TEMPUR-Adapt Pro-Adapt Made Of?
The Pro-Adapt model has multiple firmness options: Soft, Medium, and Firm, as well as a Medium Hybrid variant. All models are 12 inches thick. For hip pain, we recommend the Soft or Medium all-foam versions, so we’ll describe the construction of these two:
- SmartClimate® Dual Cover System – A cooling zip-off cover and a stretchy knit inner layer combine to create a comfortable sleep surface.
- Comfort Layer – In the softer model, it’s made up of TEMPUR-ES® material, which the brand calls its “softest material.” In the Medium model, it’s the original TEMPUR® material for a truly middle-of-the-road feel.
- Support Layer – TEMPUR-APR™ material makes up this layer in both models, designed to relieve pressure while still keeping your body lifted.
- Core – The base of the mattress is made up of dense poly foam for sturdy stability.
Our Take: Tempur-Pedic is a brand name known for providing science-backed materials and luxurious comfort. If you’re looking for that classic “hug” that comes from memory foam, you’ve come to the right mattress. The Pro-Adapt® should have that and more.
What We Liked
- Great at isolating motion – The ProAdapt® has a dense, cushiony surface that absorbs motion like a champ. Say hello to undisturbed sleep as you and your partner toss and turn to your heart’s content.
- Iconic material – Tempur-Pedic’s proprietary TEMPUR® material is perhaps what many people think when they hear the term “memory foam” in the mattress business. It’s like memory foam but better, comfortably conforming to a sleeper’s unique silhouette for unparalleled pressure relief and support.
Potential Drawbacks
- Hard bargain – This mattress is truly a luxury buy, so be aware that a queen will cost you over $3,000, making it the most expensive mattress on this list.
- Not the most responsive – All the cushiony foams won’t respond as quickly as springs. It’s possible that you might need more bounciness from your bed for especially restless legs.
Want to read more? Check out our in-depth guide to Tempur-Pedic mattresses or explore our picks for the best mattress for hip pain.
What to Look for In A Mattress for Restless Legs Syndrome
Restless legs syndrome (RLS) comes with a variety of symptoms, including discomfort in the legs and an irresistible urge to move them. With that in mind, if you have RLS you’ll want to choose a mattress that has features to help you get good quality and quantity sleep.
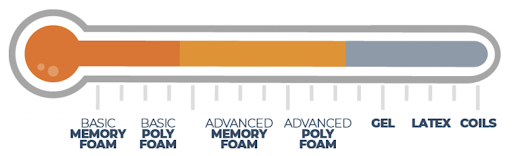
Type of Mattress

Innerspring Mattresses
Innerspring beds are sometimes the worst choice for people with RLS because of the coils inside the mattress, which create a lot of bounce. This means that whenever you move or get up, you’re affecting the springs around you. If you’re having a particularly rough night, your partner may find themselves awake right along with you, which could put stress on any relationship.
Hybrid Mattresses
Hybrid beds are a great alternative for those with RLS who love the bounce of coils but also want something that won’t disturb their partner as much.
Most hybrid mattresses contain pocketed coils, which are individually wrapped in fabric. This allows them to move independently and keep motion more isolated to one side of the bed.

Memory Foam Mattresses
A top choice for people with restless legs syndrome is a memory foam mattress. This type of foam excels at motion isolation, which means that if one partner tosses and turns, then the other person isn’t likely to be disturbed.
Latex Mattresses
Latex mattresses are naturally bouncy and sleep cool.
Despite latex’s benefits, its buoyancy means it’s not going to be the best choice for those with RLS because it’ll create more motion transfer across the bed when you move around.

Other Considerations When Shopping for a Mattress for Restless Legs Syndrome
Sleeping Position
People with RLS might have to rotate among positions to find some comfortable enough to get to sleep, or sometimes they need to leave the bed and walk around until the discomfort goes away. Once you do find something comfortable enough that you tend to gravitate toward, you can use that preferred position to help you choose a mattress.
For example, side sleepers typically do better with beds that are a bit softer and more pressure-relieving, to cradle the shoulder and hip. Stomach sleepers will do better with a firm bed to keep the spine in alignment, and back sleepers tend to need something medium-firm for balanced support and pressure relief.

Weight/Body Type of Sleepers
Body type and weight also play a role in choosing your mattress. As we mentioned before, memory foam beds tend to be the best for isolating motion, an important factor for those with RLS. That said, memory foam beds are sometimes not supportive enough for those who weigh more than 230 pounds or so. In this case, you’d probably do better with a hybrid bed, which can include both supportive springs as well as memory foam.
Lightweight and most average-weight sleepers should feel plenty supported by most mattress types, including memory foam.
Firmness
People with RLS tend to toss and turn, switching positions frequently throughout the night. While we typically recommend different mattress firmness levels depending on someone’s preferred sleeping position, this principle doesn’t necessarily apply to someone with RLS.
Because you’re tossing and turning, you may be spending time on your side, stomach, and back. Given the variety, you may do best with a mattress that universally accommodates all three. Therefore, a medium-firm bed could be an ideal choice.
Cooling
Whatever the cause, if you get hot at night, it’s important to find a mattress that keeps you cool. Memory foam is known to trap heat more than other materials, but it is also the best at isolating motion.

A good compromise is to select a memory foam mattress with cooling features like perforated foam or cooling gel or choose a memory foam hybrid bed that also has innerspring coils for added airflow.
Motion Isolation
If you have restless legs syndrome and sleep with someone nightly, you’ll want to consider a mattress that isolates motion well, such as a bed with memory foam. Anything else can run the risk of causing your partner to wake up every time you move around.
Sex
If you’re sexually active, you’ll want to choose a bed that enhances this part of your life, rather than detracts from it. A lot of people love a bouncier bed for sex, but unfortunately, a bouncier bed can be worse for those with RLS.
In this case, a good alternative would be a hybrid bed, which has more bounce than an all-foam bed but still has good motion isolation.
For More Information: Top-Rated Mattresses for Sex
Pressure Relief
Pressure relief might be an important factor for those with RLS. A bed with good pressure relief will cradle the joints and curves of your body so that your weight is more evenly distributed and no one part of your body is uncomfortably bearing any pressure.
A bed with maximum pressure relief will feel like you’re sinking down into it; a bed with minimal pressure relief will feel like you’re lying right on top of it. Finding something in the middle that works for you and keeps your legs feeling comfortable is key.

Typically, a bed that includes memory foam will be a great choice for pressure relief.
Read More: Best Mattresses for Pressure Ulcers
Edge Support
Beds with great edge support are reinforced around their perimeter, in order to keep the edges from sagging. They can either be reinforced on two sides of the bed or all four. This matters when you’re getting into or out of bed and also when you’re sleeping. If the edges of your bed begin to sag, you won’t be able to comfortably (or safely) use the entire surface of your bed.
For those with RLS, who may be moving around quite a bit at night or even getting in and out of bed more often, edge support is important. Be on the lookout for this feature in the description of your mattress.
Budget
When buying a bed, we recommend that you don’t just go for the cheapest one. Instead, try to find a mattress that is within your budget but one that is still high-quality and that comes with a good trial deal This way, you can try out the mattress, and if it doesn’t work, you can send it back for a refund.
On average, you can expect to spend about 1,000 dollars for a foam mattress, 900 dollars for an innerspring, 1,000 dollars for a hybrid, and about 1,500 dollars for a latex bed. However, this also depends on the size of the mattress, and you can usually save money by ordering your mattress online or paying attention to special holidays when mattresses go on sale.
Read More: How Much Does a Mattress Cost?
What Causes Restless Legs Syndrome?
According to the Mayo Clinic1, there’s often not a specific cause for RLS, though scientists believe it may be associated with a dopamine imbalance2.Certain things can increase your likelihood of experiencing RLS, including genetics, pregnancy (particularly during the third trimester), iron deficiency, peripheral neuropathy, alcoholism, diabetes, certain spinal cord conditions, kidney failure, and Parkinson’s disease.1
How Can a Mattress Help with Restless Legs Syndrome?
RLS can have a significant impact on sleep quality and duration3 so finding a mattress that helps keep you comfortable, relieves pressure on the legs, and minimizes motion will be important.
Though there aren’t any specific scientific studies looking at how different types of mattresses impact RLS symptoms, there is a lot of good research out there about how certain lifestyle changes can help symptoms. Some of these can be incorporated into the mattress you choose.
- It can massage the legs – According to health experts, massaging the legs4 can help relax the muscles and improve symptoms of RLS. A bed with massage features might help you sleep better through the night.
- It can help you stay cool – Night sweats appear to be associated with a variety of sleep conditions5 that disrupt sleep, such as obstructive sleep apnea. Though the nature of the associations with restless leg syndrome is unclear, trying to find a bed that keeps you cool may help you sleep more soundly. Additionally, applying hot and cold, alternately, to the legs can help with symptoms. So you may try applying a heating pad to your legs before bed, but then be sure to sleep on a mattress that is cooling.
- It can minimize nighttime disturbances – A bed that minimizes motion transfer can be especially helpful if you share a bed with somebody else. A bed with excellent motion isolation will help absorb these movements and help prevent your partner from waking up. Memory foam is the best material for absorbing motion.
- It can provide better comfort – A bed that relieves pressure on the legs may help keep you more comfortable through the night. Again, memory foam is the best material for both isolating motion and relieving pressure.
What Is the Best Sleeping Position for Restless Legs Syndrome?
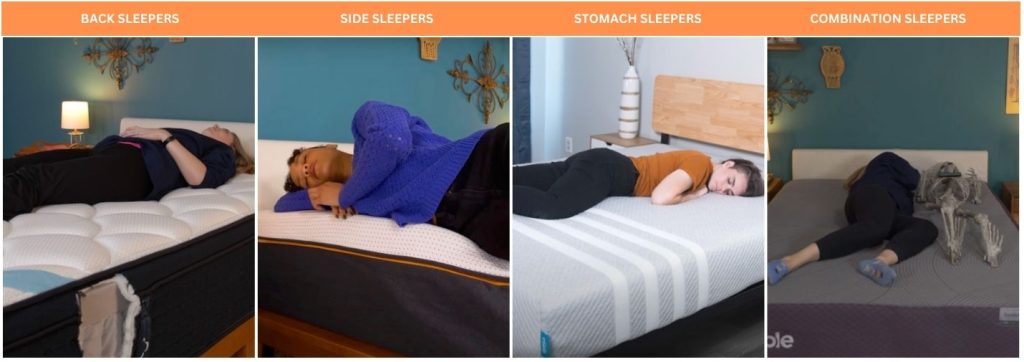
Back Sleeping
Sleeping on your back with RLS can be helpful since back sleeping evenly distributes your weight. It might also be helpful to tuck a pillow underneath your knees, to remove any discomfort from your lower back and help improve blood flow.
Read More: Best Mattress for Back Sleepers
Side Sleeping
Side sleeping is a good second option to back sleeping. Rather than sleep with your legs tucked up in the fetal position, though, try extending your legs long and placing a pillow beneath your knees. This might help the desire to move, as well as improve circulation and spinal alignment.
Plus, sleeping on the left side in particular is good for digestion, which research indicates6 may help with symptoms of RLS.
Read More: Best Mattress for Side Sleepers
Stomach Sleeping
Stomach sleeping is generally not the best sleep position for most people because it is hard on your neck and spine.
That being said, if it’s the posture that helps you get to sleep best, you just want to be sure your spine remains in as good of alignment as possible by investing in a firmer mattress and sleeping on a low-loft pillow.

Helpful Finds: Best Pillows for Stomach Sleepers and Best Mattresses for Stomach Sleepers
Combination Sleeping
It’s not uncommon for people with RLS to move from position to position throughout the night. That being said, you just need to make sure your mattress will accommodate different positions, and this in case, your best bet would be a medium-firm option.
Read More: Best Mattresses for Combination Sleepers
Tips for Better Sleeping with Restless Legs Syndrome
- Look for an adjustable bed – Adjustable beds could help you get comfortable. As mentioned, massages can be helpful for RLS, so you might also consider looking for an adjustable bed that has a built-in massage feature. If your RLS is causing pain, a little massage may offer just the relief you need.
- Try a weighted blanket – Weighted blankets can be helpful for a wide variety of ailments, including RLS. According to healthcare experts, the pressure of the weighted blanket can mask the discomfort7 associated with RLS.
- Create a regular sleep schedule – Going to bed and waking up at the same time each day helps train your body and mind when it’s time to be tired and when it’s time to wake up. Fatigue worsens RLS symptoms, so creating this routine should help.
- Avoid caffeine – Cutting out caffeine could help with RLS.4 It may sound hard, but try eliminating caffeine from your diet for a few weeks and see if it helps.
- Get moderate exercise each day – The Mayo Clinic recommends getting a moderate amount of exercise each day for RLS symptoms.4
- Take a bath before bed – A warm bath with Epsom salts may help relax your muscles and calm your nervous system.4
- Do some gentle stretching – Start and end your day with some gentle stretching.
- Up your iron intake – RLS is associated with low iron levels, so we recommend speaking with your doctor or healthcare provider to consider checking an iron panel from your blood prior to taking supplemental iron. Incorporating more iron-rich foods8 into your diet, such as spinach, seafood, whole grains, beans, and almonds can help optimize your dietary iron intake.
- Don’t drink alcohol before bed – Research shows that alcohol not only has a negative impact on sleep quality9 but more specifically, it worsens RLS symptoms10. Try abstaining from alcohol for one month and see how that impacts your sleep.
- Talk to your doctor – Your doctor may prescribe you specific medications, supplements, exercise regimens, foods, or any number of treatment options. The best way to find out what will work for you is to speak to somebody you trust and who knows your medical history.
| Mattress | Best For | Price (Queen Size) | Review |
| Helix Midnight Luxe | Combination Sleepers | $2,049 | Helix Midnight Luxe Mattress Review |
| WinkBed | Hybrid | $1,799 | WinkBed Mattress Review |
| Bear Star Hybrid | Side Sleepers | $1,998 | Bear Star Hybrid Mattress Review |
| Saatva Classic | Back Pain | $1,995 | Saatva Classic Mattress Review |
| Nolah Signature | Pressure Relief | $1,599 | Nolah Signature Mattress Review |
| Brooklyn Bedding Signature Hybrid | Back Sleepers | $1,249 | Brooklyn Bedding Signature Hybrid Mattress Review |
| DreamCloud | Luxury | $1,332 | DreamCloud Mattress Review |
| Nectar | Couples | $999 | Nectar Mattress Review |
| Loom & Leaf | Memory Foam | $2,395 | Loom & Leaf Mattress Review |
| TEMPUR-Adapt® ProAdapt® | Hip Pain | $3,199 | Pending |
Best Mattress for Restless Legs Syndrome FAQs
What’s the best sleeping position for people with RLS?
When it comes to RLS, there’s no single sleeping position that’s better than the rest. The best thing you can do is find something that’s comfortable for you and remind yourself that you might need to switch a few times (or more) during the night.
What to do if your partner has restless legs?
If your partner has restless legs, their constant movement is probably keeping you awake, too. In this case, the same rules can apply as if you were the one with RLS and in search of a new mattress.
Look for a bed that is optimized for comfort and does a great job at curbing motion transfer so you’re less likely to notice their movements.
Feel like more space would help? Consider a King size mattress or a California king mattress.
How can I manage my restless legs syndrome and start being able to fall asleep?
There are many things you can do during the day and into the night to prevent restless leg syndrome from keeping you up at night. The things that will have the biggest impact are lifestyle changes. Exercise regularly, eat a healthy diet, and cut caffeine, processed sugar, and alcohol as these have been shown to exacerbate and even cause RLS symptoms.
.

Julia Forbes
Lead Product Tester
About Author
Julia is the Lead Reviewer at Sleep Advisor, specializing in testing out mattresses and sleep accessories – she’s in the right line of work, because she loves to sleep.
Stomach Sleeper
References:
- “Restless legs syndrome”. Mayo Clinic. Last modified March 1, 2022.
- “Dopamine”. Cleveland Clinic. Last modified March 23, 2022.
- Bogan, Richard. “Effects of restless legs syndrome (RLS) on sleep”. Neuropsychiatric Disease and Treatment. 2006.
- “Restless Legs Syndrome: Diagnosis & treatment”. Mayo Clinic. Last modified March 1, 2022.
- Mold MD, James., Woolley, Joseph., Nagykaldi PhD, Zsolt. “Associations between night sweats and other sleep disturbances: An OKPRN study”. Annals of Family Medicine. 2006.
- “High levels of rare gut bacteria may be linked to restless legs syndrome”. American Academy of Sleep Medicine. 2019.
- “Do weighted blankets really work?”. Alaska Regional Hospital. 2019.
- “What to Eat If You Have Restless Legs Syndrome”. Cleveland Clinic. 2019.
- Thakkar, Mahesh., Sharma, Rishi., Sahota, Pradeep. “Alcohol disrupts sleep homeostasis”. Alcohol. 2015.
